Telehealth Website Design: Building Compliant Virtual Care Platforms



Telehealth grew from 0.3% of medical visits in 2019 to over 30% at pandemic peak. While that number has stabilized around 17%, virtual care is now permanently embedded in healthcare delivery. The infrastructure requirements are permanent too: HIPAA-compliant video, secure patient communications, EHR integration, and user experiences that work for patients accessing care from phones, tablets, and computers.
Building telehealth websites involves different technical challenges than standard healthcare sites. Video infrastructure, real-time communication, device compatibility, and integration with clinical systems add layers of complexity that most web designers don't encounter.
What Makes Telehealth Design Different
Standard healthcare websites are mostly informational: describe services, build trust, convert visitors into patients. Telehealth websites are application platforms where clinical care actually happens.
The Application vs. Website Distinction
A clinic marketing site has predictable traffic patterns and straightforward infrastructure. A telehealth platform handles: Real-time video with latency requirements under 150ms for natural conversation. Standard web hosting doesn't cut it.
Simultaneous connections during peak hours. Virtual waiting rooms need infrastructure that scales.
Multiple device types including older phones, tablets with weak cameras, and computers with various browser versions.
Intermittent connectivity from patients in rural areas or with unstable internet. The platform needs graceful degradation, not complete failure.
EHR integration writing notes, prescriptions, and orders into electronic health records in real time.
These requirements push telehealth into application development territory, not just web design.
Compliance Is More Complex
Standard healthcare websites need to protect form submissions and analytics. Telehealth platforms transmit video and audio of actual clinical encounters. The compliance requirements scale accordingly: PHI transmitted includes the entire clinical interaction: what the patient says, what the provider sees, what's discussed about symptoms and treatment. Every frame of video is PHI.
Recording considerations add storage, retention, and access control requirements if sessions are recorded for clinical purposes.
Prescription handling through telehealth involves controlled substance regulations beyond HIPAA.
Multi-state practice creates additional complexity as telehealth crosses state licensing boundaries.
Video Infrastructure Options
Doxy.me: Purpose-Built for Healthcare
Doxy.me was built specifically for telehealth with HIPAA compliance as the foundation, not an afterthought. The free tier handles basic video visits. Paid plans add features like virtual waiting rooms, call recording, and custom branding.
Strengths:
- BAA included at all tiers
- No software installation for patients (browser-based)
- Built-in virtual waiting room
- Screen sharing for patient education
- Patient queue management
Limitations:
- Limited customization options
- Video quality can struggle on slow connections
- Integration with other systems requires paid plans
Best for: Solo practitioners and small practices wanting turnkey telehealth without development costs.
Daily.co: Developer-Focused Video API
Daily.co provides video infrastructure as an API, giving developers full control over the experience. They offer HIPAA compliance with BAA on appropriate plans.
Strengths:
- Full design control over video interface
- Robust API with comprehensive documentation
- Server-side recording options
- Custom virtual waiting room implementation
- Breakout rooms for group therapy
- WebRTC-based for browser compatibility
Limitations:
- Requires development work to implement
- Pricing scales with usage (minutes)
- HIPAA tier requires custom agreement
Best for: Custom telehealth platforms needing branded video experiences or integration with proprietary systems.
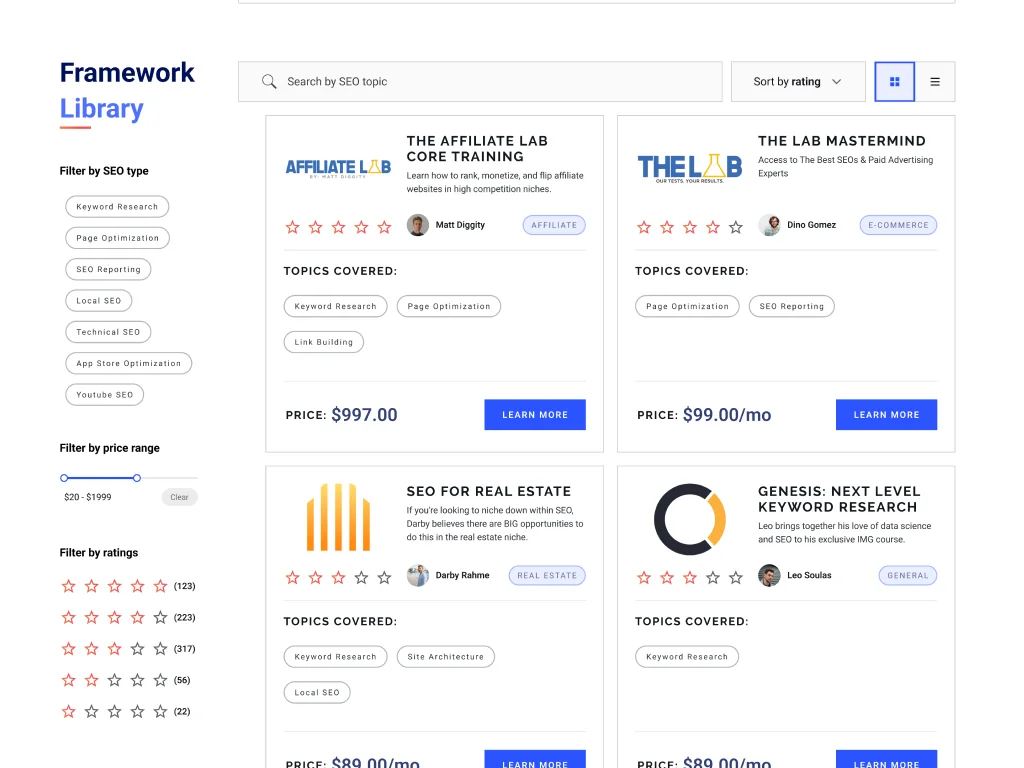
Video Platform Comparison
| Platform | HIPAA Compliant | BAA Available | Custom Branding | Development Required | Starting Price |
|---|---|---|---|---|---|
| Doxy.me | Yes | Yes (all plans) | Limited | No | Free |
| Daily.co | Yes (HIPAA tier) | Yes (enterprise) | Full | Yes | $0.004/min |
| Zoom Healthcare | Yes | Yes | Moderate | Minimal | $200/mo |
| SimplePractice | Yes | Yes | Limited | No | $69/mo |
| VSee | Yes | Yes | Moderate | No | $49/mo |
Building Custom Telehealth Experiences
When off-the-shelf platforms don't fit your clinical workflow, custom development makes sense. Common scenarios:
Specialized Clinical Workflows
Dermatology telehealth needs high-resolution image capture and comparison tools. Mental health needs different UX than physical exam workflows. Pediatrics needs interface designs that work when parents hold devices while providers examine children.
Generic video platforms don't accommodate these specialized needs without customization.
EHR Integration Requirements
If your clinical workflow requires video visits to automatically create encounter notes, pull patient history, queue prescriptions, or trigger billing codes, integration with your EHR becomes essential.
Major EHR systems provide APIs for integration: Epic offers FHIR APIs for patient data exchange and the MyChart platform includes telehealth capabilities.
Cerner (now Oracle Health) provides similar FHIR-based integration paths.
eClinicalWorks has built-in telehealth but allows external video platforms through their API.
athenahealth supports third-party telehealth integration through their developer program.
The HL7 FHIR standard provides a common language for these integrations, though implementation details vary by vendor.
Remote Patient Monitoring Integration
Telehealth extends beyond video visits. Remote patient monitoring (RPM) connects web interfaces with physical devices: Blood pressure monitors, glucose meters, pulse oximeters transmit readings that appear in patient dashboards and provider views.
Wearables like continuous glucose monitors or cardiac monitors stream data requiring real-time display.
Connected scales, spirometers, and other devices add home-based data to the clinical picture.
Web Bluetooth API enables browser-based connections to compatible devices, though many RPM implementations use dedicated apps that sync to web platforms.
UX Considerations for Virtual Care
The Virtual Waiting Room
Patients logging in early need somewhere to wait. The virtual waiting room serves multiple purposes: Technical checks verify camera, microphone, and connection quality before the visit starts.
Information display shows wait time estimates and what to expect during the visit.
Pre-visit forms capture reason for visit, symptoms, or vitals if the patient has home monitoring equipment.
Anxiety reduction for patients nervous about telehealth through clear instructions and reassuring design.
Poor waiting room UX leads to patients refreshing pages, closing browsers, or calling the clinic. Good UX keeps them engaged and prepared.
Elderly and Technology-Limited Users
Telehealth patient populations include seniors and others with limited technology comfort. Design for: Large click targets because tremors and reduced fine motor control make small buttons difficult.
Clear visual hierarchy with obvious next steps because complex interfaces confuse users.
Prominent help options including phone numbers for those who get stuck.
Browser compatibility including older browsers that some users haven't updated in years.
Mobile-first layouts because many seniors use tablets as primary devices.
Testing with actual senior users reveals usability issues that younger designers miss.
Accessibility Beyond WCAG
Standard WCAG compliance addresses visual, auditory, motor, and cognitive accessibility. Telehealth adds unique considerations: Video call accessibility for patients who lip-read (clear video quality matters), have hearing aids (audio clarity and volume control), or use sign language interpreters (multi-party video support).
Screen reader compatibility for blind patients navigating the interface before and during calls.
Cognitive accessibility for patients with conditions affecting memory, attention, or processing speed. Clear, simple interfaces reduce cognitive load.
Caption support for deaf or hard-of-hearing patients when interpreters aren't available.
Cost Structure for Telehealth Platforms
Telehealth infrastructure costs more than standard websites because you're paying for real-time communication infrastructure.
Video Platform Costs
Per-minute pricing (Daily.co model): $0.004-0.02 per participant minute. A 15-minute visit with two participants costs roughly $0.12-0.60. Volume discounts apply.
Per-seat licensing (Zoom Healthcare model): $200-300 per provider per month regardless of usage.
All-in-one platforms (SimplePractice model): $69-99 per month including scheduling, documentation, billing, and telehealth video.
Infrastructure Costs
Beyond video, telehealth platforms need: Hosting for the web application: $150-500/month for HIPAA-compliant hosting depending on traffic.
Database with encryption at rest: Included with some hosting or additional $50-200/month.
Backups and disaster recovery: Essential for healthcare, adding $50-100/month.
CDN for static assets: $20-100/month for faster page loads globally.
Development Costs
Custom telehealth development ranges widely: Basic custom implementation connecting video API to existing EHR: $15,000-40,000
Full custom platform with scheduling, video, documentation: $75,000-200,000+
Ongoing maintenance for compliance updates, security patches, feature additions: $2,000-10,000/month
For many practices, using established platforms makes more economic sense than custom development. Custom builds make sense when your clinical workflow has unique requirements that platforms can't accommodate.
My Approach to Telehealth Projects
When clients come to me with telehealth requirements, I first determine whether custom development makes sense or whether implementing existing platforms would serve them better.
Assessment Questions
Is the telehealth component your core product or an addition to existing practice? Telehealth-first businesses may need custom platforms. Practices adding virtual visits usually benefit from established platforms.
What EHR integration is required? Simple "launch external video" integration differs dramatically from "automatically write encounter notes to Epic."
What's your patient population? Tech-savvy urban millennials have different needs than elderly rural patients with limited internet.
What's the budget? Custom telehealth development costs can exceed the value it creates for many practices.
When I Recommend Existing Platforms
For most practices, I recommend SimplePractice, Jane App, or Doxy.me integrated with a custom marketing website. The practice management platform handles scheduling, video, documentation, and billing. The custom website handles patient acquisition, trust building, and brand differentiation.
This approach works because: - Video infrastructure is handled by experts in real-time communication
- HIPAA compliance is the platform's responsibility
- Development budget goes toward unique differentiators rather than reinventing video calling
- Ongoing maintenance is the platform's responsibility
When Custom Development Makes Sense
Custom telehealth development is justified when: Unique clinical workflows require features no platform provides. Specialized assessments, proprietary protocols, or multi-provider coordination patterns might need custom solutions.
Integration requirements exceed what platforms offer. If your EHR, lab systems, pharmacy network, and billing systems all need real-time integration, custom development may be necessary.
Scale and cost math favors building. High-volume telehealth operations may find per-minute video costs exceed the cost of running their own infrastructure.
Competitive differentiation depends on proprietary technology. Telehealth startups building technology as their product need custom development.
For these projects, I build on SvelteKit with Daily.co for video infrastructure. The technical architecture looks like: - SvelteKit frontend and API routes
- Daily.co video rooms embedded in the application
- Direct EHR API integration
- HIPAA-compliant hosting on AWS or Healthcare Blocks
- Real-time database for session state and messaging
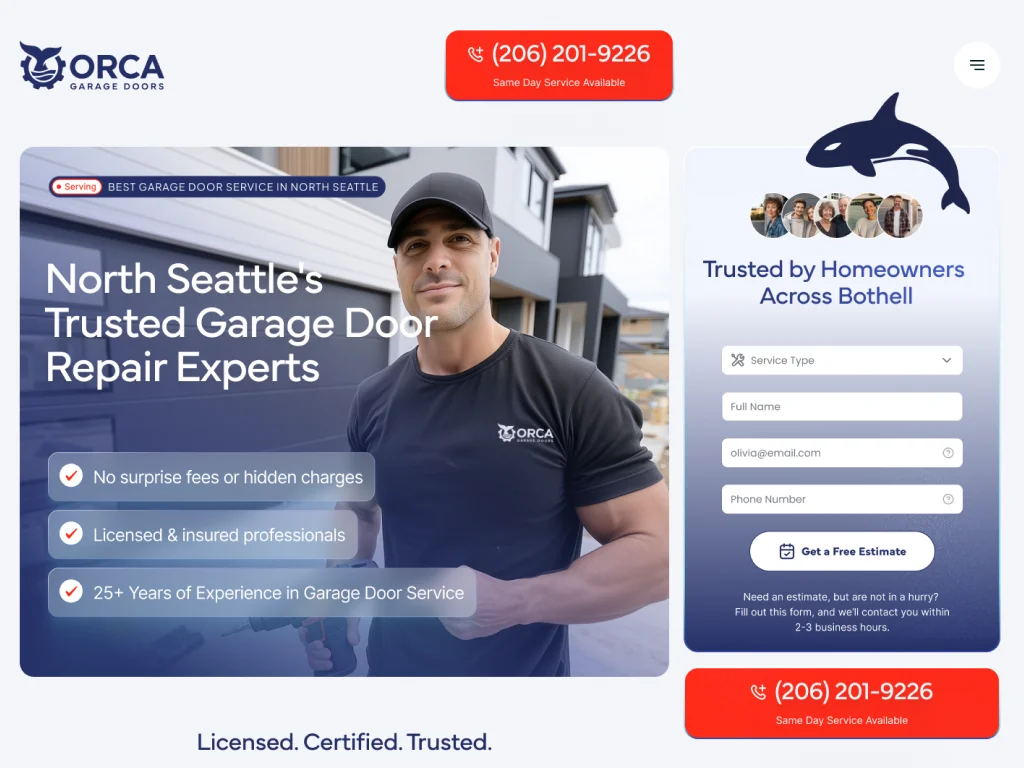
Case Study: Wellness Clinic Virtual Care
The Korawells wellness clinic project demonstrates the hybrid approach. The clinic offers in-person and virtual services. Rather than building custom telehealth, we integrated with their existing practice management platform: Marketing website built on SvelteKit handles patient acquisition and information. Custom animations and design create a memorable brand experience.
Telehealth runs through their practice management system. Patients book virtual visits through the same scheduling system as in-person appointments.
Forms use Jotform's HIPAA-compliant tier for any health-related inquiries, with autocomplete disabled to prevent browser caching of sensitive information.
No PHI on the marketing website. All clinical data lives in the practice management system with proper compliance infrastructure.
This approach gave the clinic a premium web presence while leveraging established telehealth infrastructure. Development budget went toward brand differentiation rather than reinventing video visits.
Getting Started with Telehealth Web Design
I work with clinics, therapists, telehealth platforms, wellness coaches, hormone optimization experts, and longevity practitioners across the US, Canada, UK, and Australia. Whether you need a custom solution or strategic implementation of existing platforms, I can help you navigate the technical and compliance landscape.
Transform your website into a revenue-generating asset
Partner with an award-winning Filipino web designer delivering world-class websites to global brands. 15+ years of experience creating sites that convert visitors into customers.
Frequently Asked Questions
-
Technically yes, but practically it's more complex. You need a HIPAA-compliant video platform, proper BAA documentation, and user flows for pre-visit preparation, virtual waiting, and technical troubleshooting. Simply embedding a video link doesn't create a good telehealth experience.
-
Good telehealth platforms handle connection issues gracefully: automatic reconnection attempts, phone backup options, and session state preservation. Patient-side you want clear instructions on what to do if disconnected. Provider-side you want visibility into connection quality before issues become critical.
-
Yes. Your BAA with your hosting provider covers your website infrastructure. Video platforms are separate business associates requiring their own BAAs. Platforms like Doxy.me include this automatically; others require negotiation at enterprise tiers.
-
Your website should clearly communicate which states you're licensed to practice in. Booking systems should verify patient location. Some practices use geo-blocking to prevent scheduling from states where they're not licensed.
-
Minimum 1.5 Mbps for acceptable video quality, 3+ Mbps recommended. Your platform should test connection quality before visits start and provide fallback options (audio-only, phone bridge) when video quality is insufficient.
-
Recording requirements vary by state, insurance requirements, and clinical context. If recording, you need patient consent, secure storage meeting HIPAA requirements, defined retention policies, and access controls limiting who can view recordings.